Hamlet (community) health workers in Vietnam learn to interact with mCare (Photo credit: FHI360)
With international development program cycles often having a “project design phase”, how can online learning as a team improve project design?
How do you design a technology program intervention to improve health outcomes?
HIV Challenges and Keeping Up with mHealth
According to the WHO, HIV has claimed 39 million lives so far globally with 1.5 million lives in 2013 alone. At the end of 2013, there were 35 million people living with HIV, with 2.1 million becoming newly infected. With 24.7 million people living with HIV in 2013, Sub-Saharan Africa is the most affected region in the world accounting for almost 70% of the global HIV infections.
HIV often gets highlighted as a major problem in Sub-Saharan Africa, but it is also a major public health concern in Southeast Asia, particularly in Vietnam where the use of needles to inject drugs drives the epidemic. As of 2012, 260,000 (of the 89 million) people in Vietnam are living with HIV, according to UNAIDS Vietnam. As a result, FHI 360 is working with the Government of Vietnam to address the country’s HIV challenges with “effective programs that cost less, are implemented locally, and decrease donor dependence”.
Technology developments in public health change very quickly, especially with the emergence of mHealth – there’s more mHealth programming, new applications, and emerging research.
MHealth is a key strategy for us as these applications can be used to incentivize health-seeking actions, increase the timeliness of data collection, improve patient communications, and document system-client interactions. MHealth can also facilitate workforce development through task shifting, performance support, and human resources management.
According the blog Tech in Asia, “For every 100 Vietnamese people, there’s 145 mobile phones. For a country whose population is just over 90 million, that amounts to more than 130 million mobile phones.” RefWorld.org reported that, as of January 2012, census data indicated there were 119 million mobile users in Vietnam when the population was at 88 million. Given the emergence of the mHealth industry and the large percentage of the Vietnamese population with cell phones, we at FHI 360 need to effectively mobilize this ubiquitous technology for impactful programming that helps individuals in all areas of the country protect their health and well-being.
A Social Online Learning Solution
In 2012, I first participated in TechChange’s 4-week online certificate course called “Mobile Phones for Public Health.” I decided to take the course again in 2013 – this time with numerous colleagues — to share our mHealth programming experiences and to continue to learn from renowned mHealth practitioners around the world.
Like all busy development professionals, it is difficult to find time to cultivate learning during our day-to-day work. The TechChange course was structured and delivered to meet our needs.
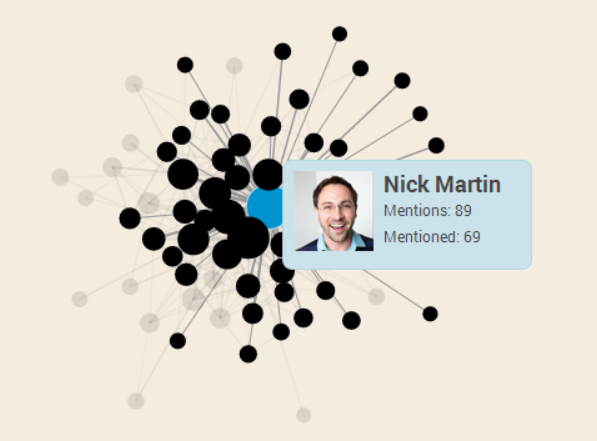
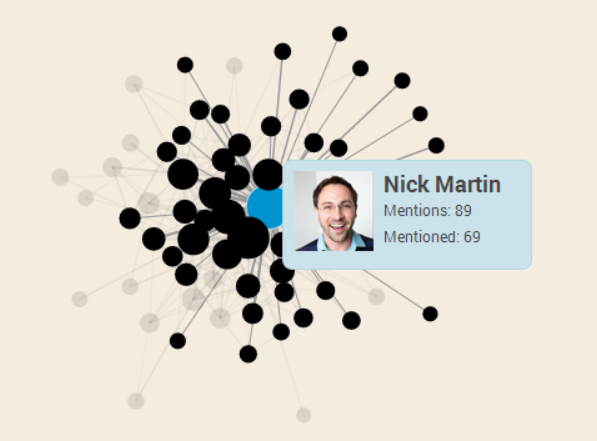
Here’s a social graph from Mobile Phones for Public Health showing participant interaction
Cutting-edge, timely, and relevant information
- TechChange updated its courses at least once every 3-6 months, based on direct feedback (through crowdsourcing and surveys) from its broad learning community to deliver the most up to date and relevant course content.
Great format for busy working professionals in Vietnam and beyond
- Keeping our busy schedules in mind, the course content was designed to be mobile and tablet-friendly, allowing us to learn wherever and whenever fit our schedules. All live events were recorded so that learners could access materials according to their schedules.
- For those of us who had difficulty finishing the course in the one-month period, access (and technical support) is available for four months after the end of the course so that we can complete our final project and receive the formal certificate.
- The online interface was the most intuitive learner platform we have ever used: An online course map visually illustrated all components of the program, while a calendar highlighted a variety of live discussion events with renowned experts from around the world.
- The main facilitator actively participated in all discussion boards; introduced weekly themes (through video, email and platform) and summarized (through print and video) the highlights of each week. He and a facilitation team also provided “office hours” for those who needed extra support (and this support was provided in various time zones).
Interactive learning experience
- There was great communication between facilitator and learners. The course required 7-9 hours of effort per week and the 50 or so participants were motivated to actively participate. Learner outcomes were clearly defined and each week’s themes were well-articulated so that we knew what to expect and what was expected from us.
- Instead of relying primarily on print materials, sharing video, audio and weekly live events/”chats” allowed learners from various cultural backgrounds to gain knowledge and skills through a variety of channels through interactive learning.
- Practical exercises and interactive simulations ensured knowledge application and exchange.
- Individuals got to know each other through a variety of “get to know you” activities and collaborative exercises.
- TechChange added some fun by integrating game dynamics into the course, awarding points each time a person participated in a discussion or attended an event, with a minimum participation threshold established in order to earn a certificate.
Joining a professional network and community
- All learners also became TechChange alumni upon finishing the course. We are now connected through social media with others in mHealth (and offered substantial discounts on upcoming courses).
- It’s been great to see other mHealth alumni like Lauren Bailey making strides in the field after joining this course.
Here are some additional comments from two of my colleagues:
“I really enjoyed reading the forums at my own pace. I liked that other participants put so much thought into them.” – Deen Gu
“I like the discussion parts most as they offer me many interesting thoughts and experiences of TechChange’s members on different topics.” -Nguyen Thi Van Anh
As a recent graduate of TechChange’s courses, I can speak to the benefits of participation.

USAID/SMART TA team provides hands-on training to hamlet health worker in Nghe An (Photo credit: FHI360)
Results of mHealth Training with TechChange
Through this mHealth course, my team learned best practices as a group to explore ways to implement mHealth projects. My colleagues learned how mobile technologies are being used in other countries and sectors and thought about ways it could be applied in Vietnam. The individuals who have participated in the TechChange course are now our office mHealth champions and are actively identifying areas of work where mHealth solutions can be applied.
Here are two current mHealth pilots we have launched in Vietnam through the USAID/SMART TA program to address HIV challenges:
1. Fansipan Challenge – uses the metaphor of Fansipan mountain (Vietnam’s highest peak), gamification, and mobile technologies to support people who inject drugs and their intimate partners to test for HIV and be linked to care if they are positive.
Fansipan was created by USAID funded SMART TA project in Vietnam. Learn more about SMART TA here.
Here is a Prezi presentation explaining the Fansipan project in Vietnam called How Mobile Technologies and Gaming are Improving HIV Program
2. mCare – is the first case management application in Vietnam that utilizes mobile technologies to support and track clients across the cascade of HIV outreach, testing, care and treatment services. It also manages performance-based incentives for hamlet health workers who identify potential clients, encourage them to test for HIV, and support them to enroll and be re-engaged in HIV care and treatment and methadone maintenance treatment.

A confirmation message sent from mCare (Photo credit: FHI360)
The Results of the mHealth Pilots So Far
While mCare is in its early stages of deployment and refinement, the Fansipan Challenge has shown a dramatic reduction in programmatic unit costs, combined with significant increases in testing uptake and HIV yield among underserved key populations. Between June – November 2013, 62% of 656 injecting drug users and their intimate partners tested for HIV after a single contact. Approximately 71% of these individuals were first time testers; 17.8% were diagnosed as HIV positive. Comparative expenditure analyses of USAID/SMART TA-supported outreach services show a 50% reduction in costs associated with identifying an HIV positive person. And preliminary data further suggest that HIV positive people identified through Fansipan have higher CD4 levels (average 287.5 cells/mm3) and will thereby have better treatment outcomes than those who initiate treatment when they are severely immuno-compromised.
These new initiatives rely on mobile technologies and we, like other technical assistance providers in the development sector, need to be constantly learning about mHealth innovations, and emerging knowledge and applications. The TechChange mHealth class was a great investment in having my team become more familiar with mHealth as we introduced our mHealth initiatives.
About Caroline Francis

Caroline Francis is FHI360’s Deputy Country Director in Vietnam and completed TechChange’s Mobile Phones for Public Health course in 2012 and in 2013 when she took the course again with her team in Hanoi and Ho Chi Minh City. She is currently involved in FHI360’s Sustainable Management of the HIV/AIDS Response and Transition to Technical Assistance (SMART TA) project in Vietnam and her areas of expertise include HIV and AIDS prevention and care and Social and behavior change communications. Caroline has previously worked as the Associate Director (HIV Prevention, Mitigation, Strategic Behavioral Communications and M&E) and Deputy Director for FHI 360 Cambodia. She received her M.A. in Anthropology from University of Victoria.